APA Style
Seok-Jun Hwang, Hyunsuk Choi, Dong-Ho Kwak, Dong-Seok Sohn. (2025). The Effect of Demineralized Autogenous Tooth Block Bone on Lateral Sinus Augmentation: A Retrospective Study. Biomaterials Connect, 2 (Article ID: 0017). https://doi.org/10.69709/BIOMATC.2025.128332MLA Style
Seok-Jun Hwang, Hyunsuk Choi, Dong-Ho Kwak, Dong-Seok Sohn. "The Effect of Demineralized Autogenous Tooth Block Bone on Lateral Sinus Augmentation: A Retrospective Study". Biomaterials Connect, vol. 2, 2025, Article ID: 0017, https://doi.org/10.69709/BIOMATC.2025.128332.Chicago Style
Seok-Jun Hwang, Hyunsuk Choi, Dong-Ho Kwak, Dong-Seok Sohn. 2025. "The Effect of Demineralized Autogenous Tooth Block Bone on Lateral Sinus Augmentation: A Retrospective Study." Biomaterials Connect 2 (2025): 0017. https://doi.org/10.69709/BIOMATC.2025.128332.
 ACCESS
Research Article
ACCESS
Research Article
Volume 2, Article ID: 2025.0017

Seok-Jun Hwang
goldhoney95@naver.com

Hyunsuk Choi
hschoi@cu.ac.kr

Dong-Ho Kwak
Kwakdental@hanmail.net

Dong-Seok Sohn
dssohn@cu.ac.kr
1 Department of Dentistry and Oral and Maxillofacial Surgery, Daegu Catholic University Medical Center, Daegu 42472, Republic of Korea
2 Department of Dentistry and Prosthodontics, Daegu Catholic University School of Medicine, Daegu 42472, Republic of Korea
3 Kwak’s Dental Hospital, Daegu 42680, Republic of Korea
* Author to whom correspondence should be addressed
Received: 30 Mar 2025 Accepted: 10 Jul 2025 Available Online: 11 Jul 2025 Published: 25 Aug 2025
When placing implants in the posterior maxilla, sinus floor elevation is often required due to insufficient alveolar bone volume. During the sinus augmentation procedure, the Schneiderian membrane is elevated, and the newly created space is filled with bone graft materials. Among various graft materials, autogenous bone is considered the most biologically suitable. However, harvesting autogenous bone can cause donor site morbidity and postoperative discomfort. Block-type autogenous tooth grafts are derived from the patient’s extracted teeth. It offers the biological stability of traditional autogenous bone while minimizing disadvantages, such as donor site risks and postoperative discomfort. Due to these advantages, block-type autogenous tooth grafts have been widely studied. We evaluated maxillary sinus augmentation outcomes using block-type autogenous tooth bone grafts in 18 patients (at Daegu Catholic University Dental Hospital) from April 2017 to October 2022. The extracted teeth were processed by creating micro-holes and demineralizing them in 0.6 N HCl for 30 minutes to produce the graft material. A lateral bony window was created using a piezoelectric surgical device, and the sinus membrane was elevated. Implants and the block-type tooth grafts were placed in the created space, and the lateral window was repositioned to complete the procedure. Postoperative clinical evaluation and radiographic analyses were conducted to assess the amount of sinus membrane elevation, gain in alveolar bone height, and osseointegration of the implants. The results demonstrated that the alveolar bone height increased in proportion to the size of the block-type graft and showed long-term stability. Even in cases of sinus membrane perforation, no postoperative complications or implant failures were observed. This study suggests that maxillary sinus augmentation using block-type autogenous tooth bone grafts offers excellent osteoinductive potential and biocompatibility, making it a highly favorable option for both clinicians and patients.
The widespread use of dental implants in edentulous areas has increased the need for complex surgical procedures to enhance available bone volume. Implant surgery in the posterior maxilla presents challenges due to a thin and low alveolar ridge, poor bone quality, and increased pneumatization of the maxillary sinus [1,2]. Implant failure in the maxillary molar region is often associated with inadequate residual bone height, insufficient ridge width, and poor bone quality [3,4]. To overcome these limitations, maxillary sinus augmentation has been widely adopted to increase bone height in the posterior maxilla [5]. There are various surgical methods for elevating the maxillary sinus. The lateral window technique involves creating an opening in the lateral sinus wall to provide direct visualization and access for instrumentation [6]. The transcrestal approach is a more conservative method that involves elevating the sinus floor through the implant bed [7]. The Caldwell-Luc operation is a traditional method that involves making an incision in the lateral wall of the sinus and elevating the Schneiderian membrane to insert bone grafts [8]. The Minimal Invasive Sinus Elevation (MISE) is a recently developed technique that reduces the risk of membrane perforation and increases implant success rates [9]. The sinus intrusion osteotomy technique involves elevating the Schneiderian membrane while simultaneously inserting bone grafts. The piezoelectric osteotomy uses ultrasonic waves to cut bones, allowing for more precise incisions [10]. These methods each have their advantages and disadvantages, and the choice depends on the patient’s condition and desired outcome. In the lateral approach, bone graft materials are used to fill the space created beneath the elevated Schneiderian membrane. A variety of grafts are employed, including autogenous, allogenic, xenogenic, synthetic bone, and combinations thereof. These materials promote bone regeneration and support the Schneiderian membrane, ensuring a stable environment for dental implants. Graft selection depends on clinical requirements, availability, and the intended regenerative outcome [11]. However, challenges related to graft materials persist. These include unpredictable resorption, the limited availability and donor site requirements of autogenous bone, the inability of alloplastic materials to promote bone regeneration, and the slow resorption rate of xenografts [12]. Additionally, a substantial volume of graft material is required for sinus augmentation. On average, 5–6 cc of autogenous bone is needed per sinus cavity, while combination graft materials require approximately 2–3 cc per site [13]. To address these limitations, some studies have explored the potential of using a patient’s blood or platelet-rich plasma (PRP) to facilitate bone formation without additional graft materials [14,15]. While previous research has reported favorable bone regeneration in the absence of bone grafts, there is limited long-term follow-up data on grafted sinus augmentation cases [16]. When sinus augmentation is performed without bone grafts, significant shrinkage of the augmented space is often observed. Therefore, this study investigates demineralized autogenous tooth block bone as a potential solution to the challenges associated with other graft materials [17]. Recently, graft materials derived from teeth have been frequently used in both alveolar bone and sinus augmentation procedures [18,19]. Demineralized autogenous tooth block bone shows great potential as a bone graft material. These grafts are prepared from extracted teeth, including recently removed third molars and teeth removed due to periodontal or endodontic disease [20]. Prior research has indicated that human teeth exhibit biocompatibility and possess both osteoinductive and osteoconductive characteristics [21]. As mentioned above, tooth block bone grafts are of particular interest because they naturally contain osteoinductive growth factors and a collagen-mineral matrix similar to alveolar bone, potentially enhancing bone regeneration and biocompatibility compared to other graft materials. Therefore, this retrospective study evaluates the effectiveness of using demineralized autogenous tooth block bone for sinus augmentation through the lateral approach in cases with limited residual bone height. This study aimed to evaluate the safety and effectiveness of tooth block bone material as an alternative for achieving bone height gain, ensuring implant success, and minimizing postoperative complications.
2.1. Patient Selection This retrospective study analyzed 18 patients who underwent implant treatment with maxillary sinus augmentation at the Department of Dentistry, Daegu Catholic University Hospital, Republic of Korea, between 2017 and 2022. The study was approved by the Institutional Review Board of Daegu Catholic University Medical Center (IRB Approval No. CR-22-174-L). Before surgery, all patients received an explanation of the procedure and provided written informed consent. Each patient’s medical history was thoroughly reviewed before inclusion, and individuals with conditions affecting bone metabolism were excluded. Smokers were not excluded from the study, but they were informed that smoking could negatively affect the implant and sinus augmentation procedure. All selected patients were free of surgical contraindications. The procedure was performed using a standardized surgical approach in the maxillary premolar and molar regions of partially or fully edentulous patients. Implant mobility was the primary criterion for determining implant failure, which was defined as the need for implant removal. The survival rate was evaluated based on the duration from implant placement to either the final follow-up or the occurrence of implant failure. Preoperative radiographic evaluations were conducted to analyze sinus conditions and residual bone height. Panoramic radiographs (Point HD; PointNix, Seoul, Korea) and cone beam computed tomography (CBCT) scans (ImplaGraphy; Vatech, Gyeonggi-do, Korea) were used for preoperative assessment and postoperative evaluation of bone gain. Residual bone height was measured in millimeters using dedicated software, and the maxillary sinus width was recorded at its broadest point. Since the Schneiderian membrane may collapse in the absence of tenting material, the extent of membrane elevation was determined by measuring the distance from the original sinus floor to the highest point of the grafted bone. 2.2. Preparation of Autogenous Tooth Block Bone Extracted maxillary premolar and molar teeth were converted into demineralized autogenous tooth block bone. The preparation involved sectioning the extracted tooth along its longitudinal axis using a disk, followed by the creation of multiple micro-holes with a round carbide bur to enhance blood penetration. The tooth block underwent demineralization for 30 min with 0.6 N hydrochloric acid in a vacuum-ultrasonic system (Vacua-Sonic System, CosmoBioMedicare Co., Seoul, Republic of Korea). Then, the tooth block was sterilized using a peracetic acid ethanol solution in a specialized device equipped with vacuum compression and ultrasonic vibration. After sterilization, the demineralized dentin-derived matrix particles were washed with phosphate-buffered saline (PBS), treated with a sterilization reagent, and rinsed with it, along with distilled water. 2.3. Surgical Protocol All patients followed the same pharmacologic protocol for prophylactic antibiotic administration. The routine prescription included amoxicillin sodium (Augmentin; Ilsung Pharmaceutical, Seoul, Korea) 500 mg, taken three times daily from one day before surgery until seven days after surgery. Additionally, a single intravenous dose of amoxicillin sodium (Amocla; Kunil Pharm, Seoul, Korea) 1 g was administered one hour before surgery. Local anesthesia was administered via a posterior superior alveolar nerve block using 2% lidocaine containing 1:100,000 epinephrine. The alveolar crest and the lateral wall of the maxillary sinus were uncovered by full-thickness mucoperiosteal flap reflection. To create the lateral window, a piezoelectric device (Surgybone; Silfradent, Sofia, Italy) equipped with a thin saw tip (S-Saw; Bukboo Dental, Daegu, Korea) was used under continuous saline irrigation (Figure 1A,B). The anterior vertical osteotomy line was positioned 3 mm posterior to the anterior sinus wall, while the distal osteotomy line was created approximately 15 mm posterior to the anterior vertical line. The vertical osteotomy height measured around 10 mm. The osteotomy design consisted of anterior and inferior cuts angled at 45° to the lateral sinus wall, whereas the superior and posterior osteotomies were made perpendicular to the lateral wall. This trapezoidal configuration facilitates repositioning the bony window to its original location after surgery (Figure 1C). The bony window was carefully separated from the maxillary sinus wall. The exposed Schneiderian membrane was then gently elevated using a flat sinus lift instrument (Figure 1D). The sinus membrane was continuously lifted until the medial and posterior walls of the maxillary sinus were exposed, after which implant placement was performed simultaneously (Figure 1E). The prepared demineralized autogenous tooth block bone was applied to the space between the apex of the placed implant and the elevated Schneiderian membrane. This helps to maintain the Schneiderian membrane elevation (Figure 1F). The bony window, once detached from the sinus wall, was repositioned to its original location. The process helps prevent soft tissue infiltration into the sinus space and promotes new bone formation (Figure 1G). Polytetrafluoroethylene sutures (Cytoplast; Osteogenics Biomedical, Lubbock, TX, USA) were used to suture the flaps with a combination of continuous locking and interrupted suturing techniques to ensure passive primary closure (Figure 1H). Postoperative instructions included avoiding nose blowing for two weeks and preventing forceful sneezing or coughing with a closed mouth. Antibiotic prophylaxis continued for one week postoperatively, and sutures were removed two weeks after surgery. After surgery, panoramic radiographs and dental cone beam computed tomography (CBCT) scans were taken to assess the surgical procedure. A healing period of 6 to 8 months was observed for osseointegration before the second-stage procedure. Before this phase, additional CBCT scans were performed (Figure 2).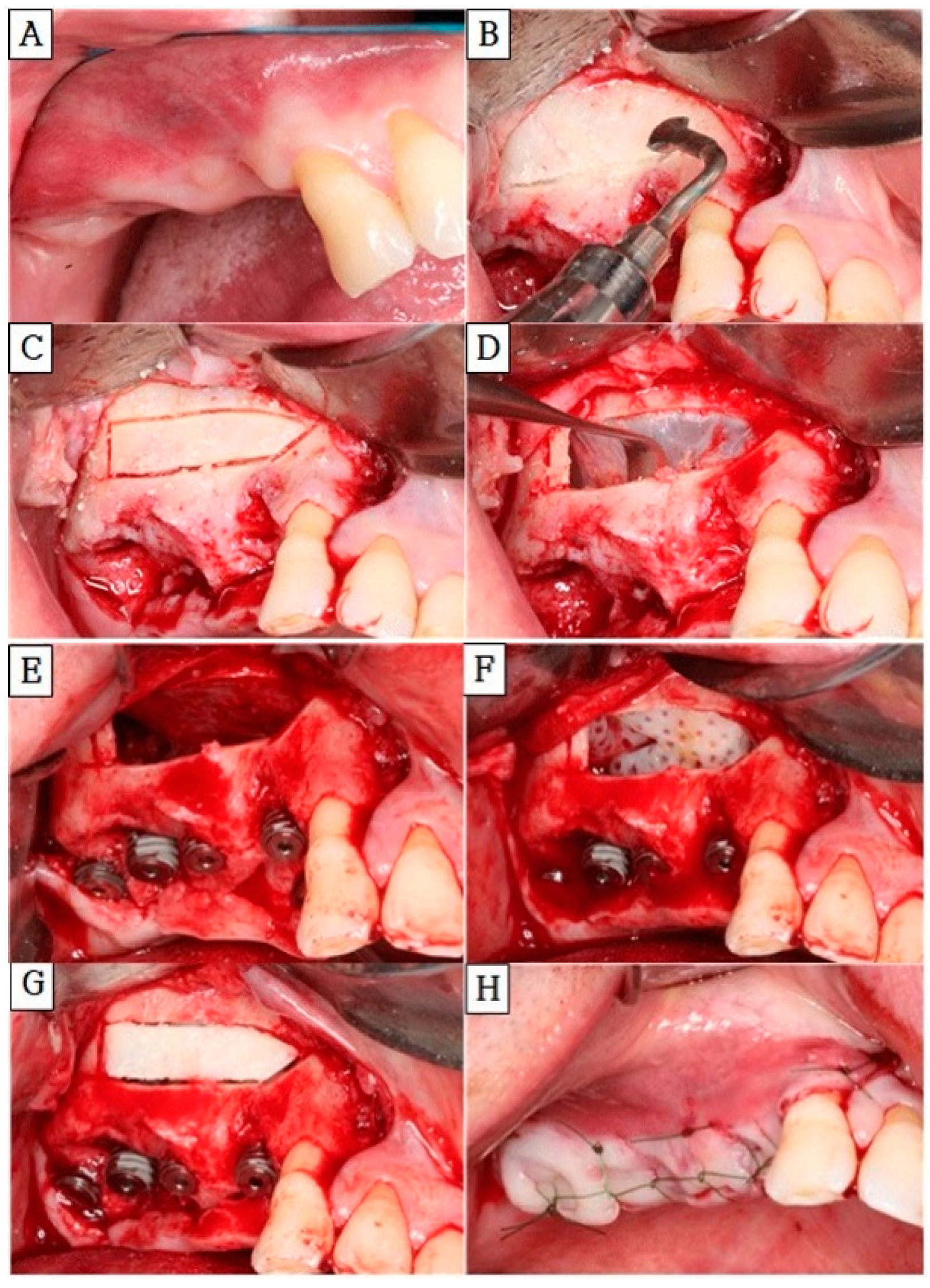
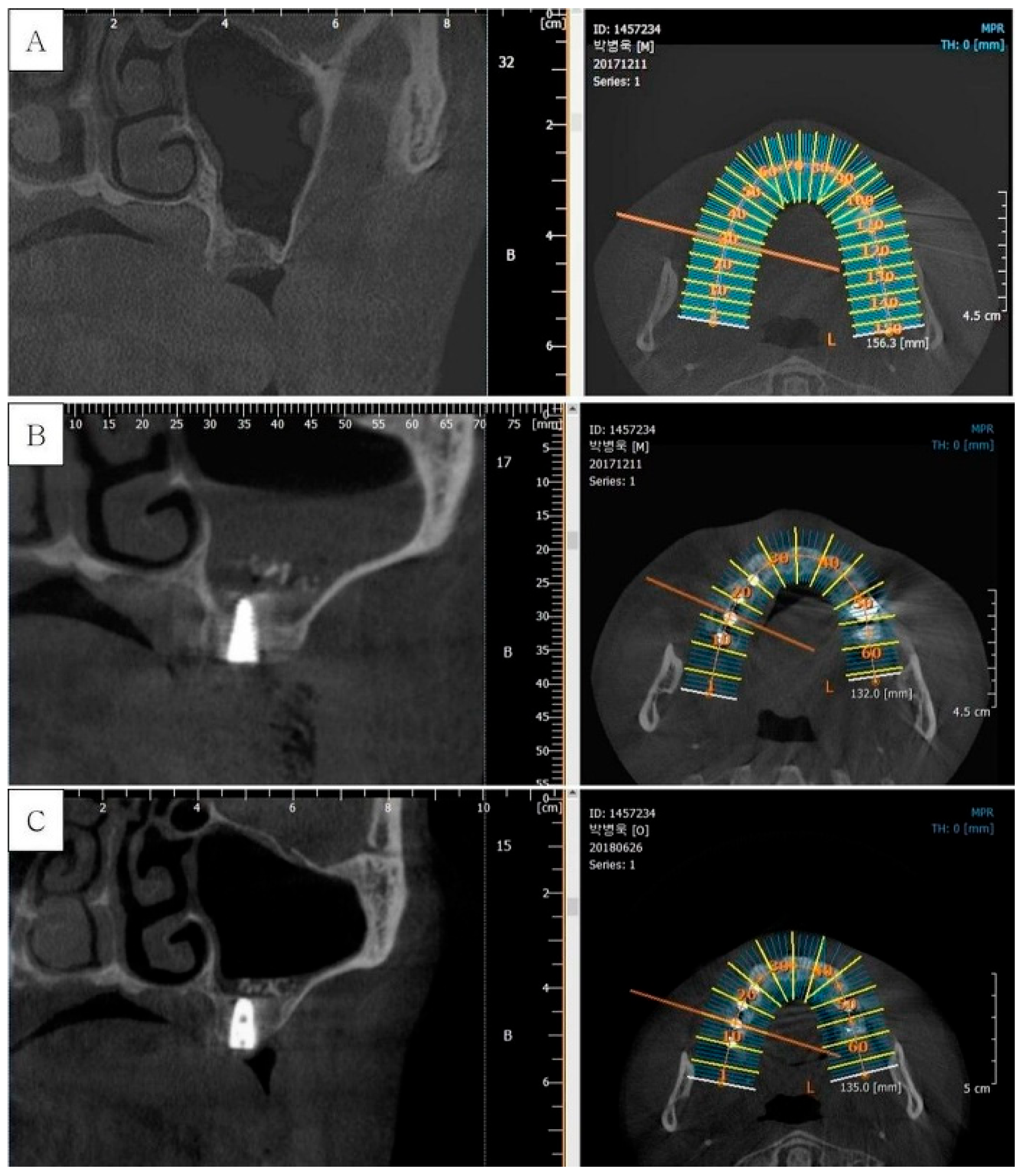
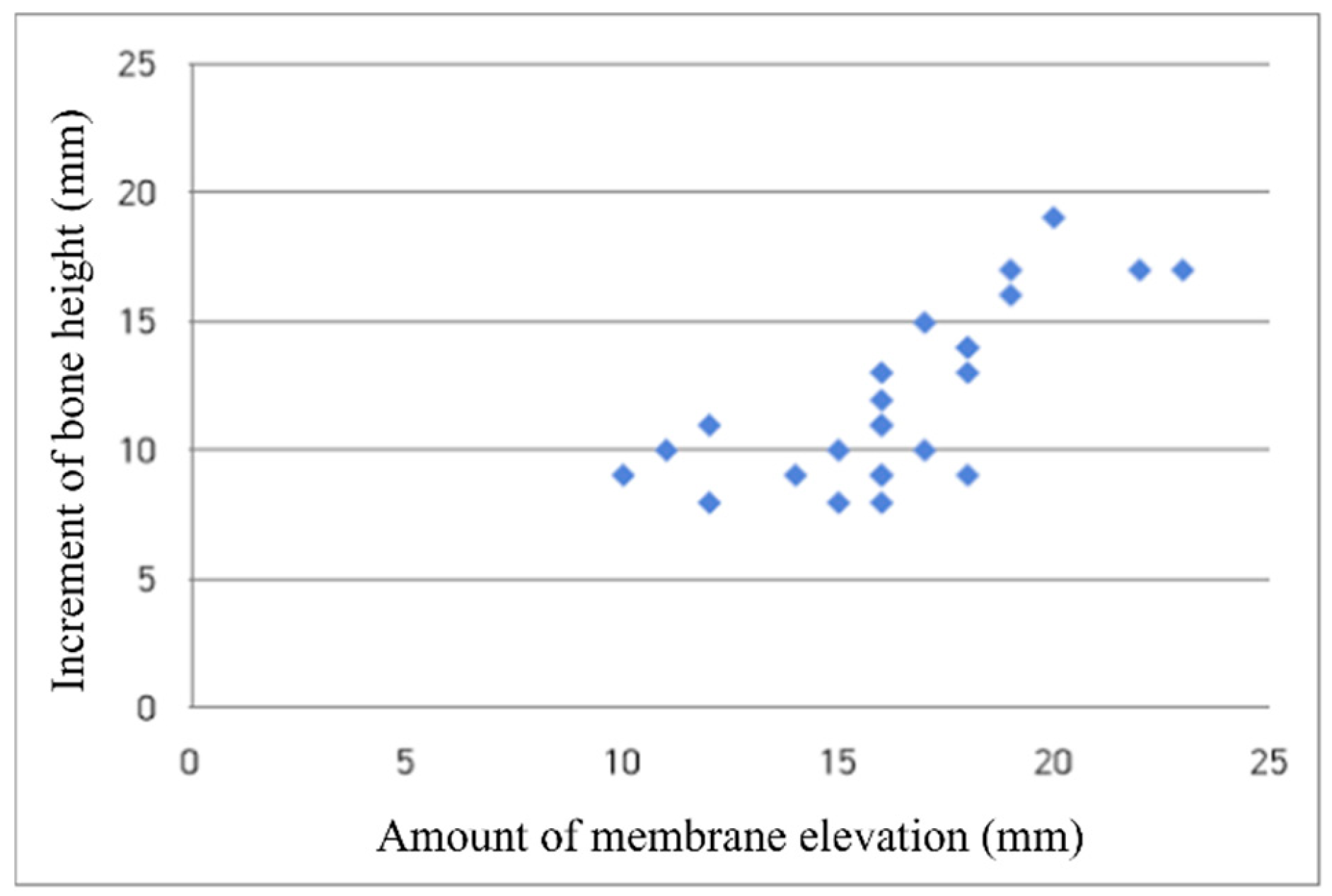
3.1. Clinical Results A total of 18 patients (11 males and 7 females) with a mean age of 53.7 years participated in this study, and all patients attended follow-up visits without any dropouts. Sinus augmentation was performed bilaterally in one patient and unilaterally in 17 patients, resulting in a total of 19 Schneiderian membrane elevation procedures and 25 implant placements. During the follow-up period, apart from mild swelling at the surgical site during the early postoperative phase, no significant complications were reported. Additionally, none of the patients exhibited an infection or sinus-related disease. Schneiderian membrane perforations, each measuring less than 3 mm, were encountered in three cases during the sinus elevation procedure. These perforations were successfully managed using absorbable collagen material (CollaTape; Zimmer Dental, Carlsbad, CA, USA). The overall implant survival rate was 100%, with no instances of implant mobility throughout the study. These findings suggest that minor Schneiderian membrane perforations had no adverse impact on clinical outcomes. 3.2. Radiographic Results Radiographic evaluation in this study consistently demonstrated a significant increase in alveolar bone height and stable new bone formation around implants following sinus augmentation with demineralized autogenous tooth block bone (Figure 3). Notably, the newly formed bone maintained its height and density during the follow-up period, with no evidence of marginal bone loss or sinus pathology on panoramic and CBCT images. These findings suggest that the tooth block graft provided effective space maintenance and osteoconductive support, likely due to its physical stability and biological compatibility. Importantly, the data revealed a positive correlation between the extent of Schneiderian membrane elevation and the amount of new bone formation, while preoperative bone height and sinus width did not significantly affect bone gain (Figure 4), (Table 1). This indicates that, within the study’s parameters, the success of bone regeneration was more closely related to the surgical elevation achieved than to initial anatomical limitations. The absence of radiographic complications such as sinusitis or graft resorption further supports the safety and predictability of this approach. These radiographic outcomes are in line with previous studies, which have shown that autogenous tooth-derived grafts can provide both structural support and biological stimulation for bone regeneration. Radiographic assessment of the maxillary sinus and alveolar crest.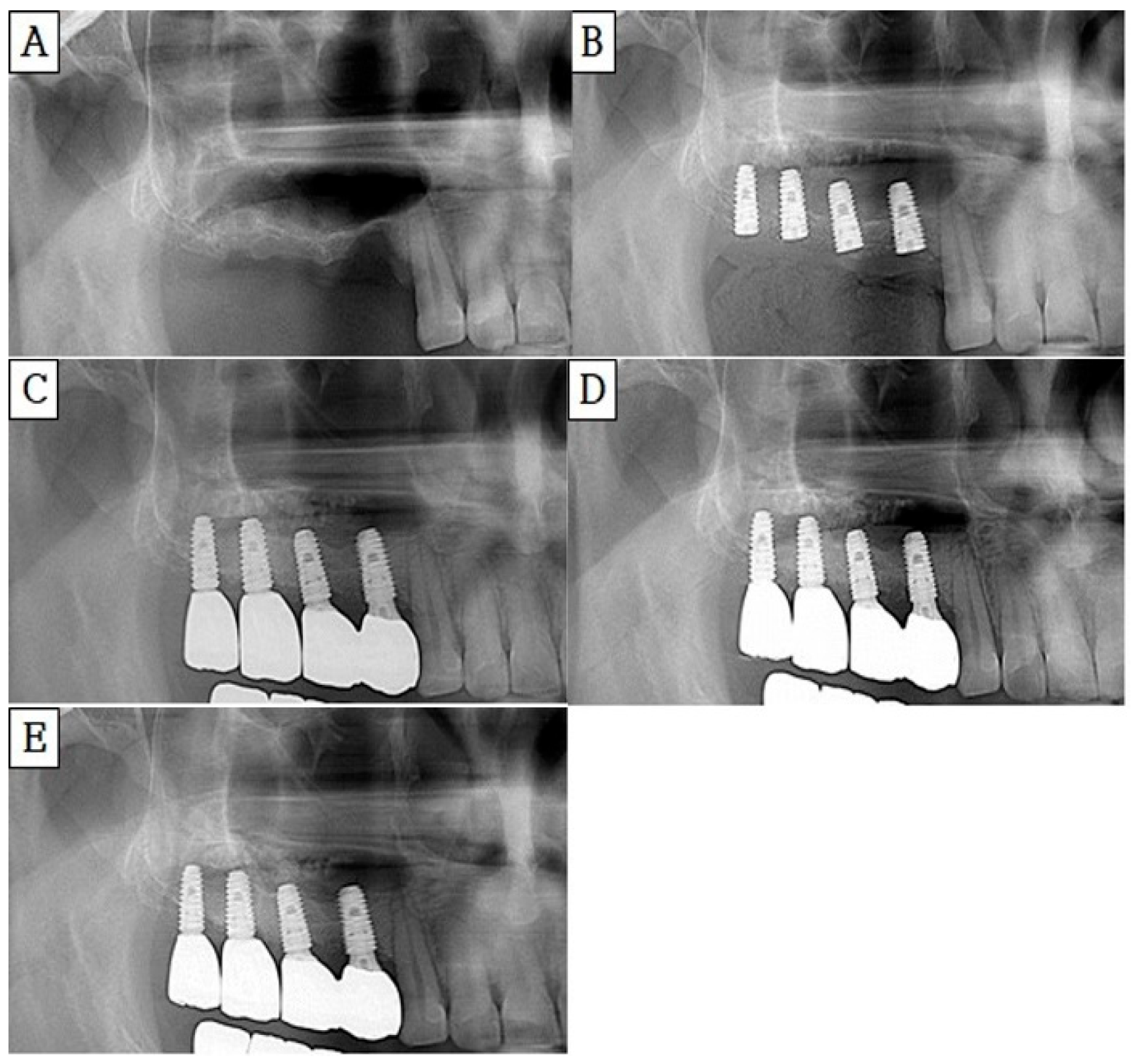
Subject
Sex/Age
Region
Schneiderian Membrane Perforation
Pre-Operative Bone Height (mm)
Amount of Membrane Elevation (mm)
Increment of Bone Height (mm)
1
M/50
#16
No
5
18
9
2
M/46
#26
No
3
17
10
3
F/50
#27
No
5
16
9
4
M/46
#14
No
5
15
10
#15
No
3
18
13
#16
No
5
14
9
#17
No
5
16
8
5
M/59
#26
No
4
16
11
#27
No
4
16
8
6
F/57
#26
No
6
18
14
7
F/52
#17
Yes
2
16
13
8
F/52
#27
No
2
19
16
9
M/65
#16
Yes
2
16
12
10
M/50
#16
No
3
23
17
#26
No
3
20
19
11
F/58
#26
No
3
19
17
#27
No
2
18
14
12
F/47
#27
No
4
16
11
13
M/64
#16
No
5
14
9
14
M/75
#26
No
4
12
8
15
F/54
#16
No
1
22
17
16
M/45
#17
No
5
17
15
17
M/52
#26
No
6
10
9
#27
No
6
11
10
18
M/45
#27
No
3
12
11
In areas with a thin maxillary alveolar ridge, it is important to perform simultaneous sinus augmentation and implant placement during implant surgery. This approach helps maintain a stable graft volume, reduces the number of surgical procedures, shortens the overall healing period, and minimizes treatment costs [22]. The conventional lateral approach for sinus augmentation utilizes powder-type graft materials derived from various bone sources. This method allows direct access to the sinus floor and is known for its predictability and simplicity [23]. However, it requires a large volume of graft material and carries a risk of sinusitis if the graft particles penetrate the Schneiderian membrane due to membrane perforation [24]. There have been several studies reporting successful sinus augmentation using only PRP and peripheral blood without the use of bone graft materials. Moon et al. performed lateral sinus augmentation without any bone graft materials, using only peripheral venous blood in 14 patients [25]. As a result, 2 out of 31 implants failed, showing an implant success rate of 93.5%. The failed cases were also associated with poor primary stability or immediate placement after extraction [25]. Therefore, the effectiveness of peripheral venous blood was demonstrated. There has been another study in which sinus augmentation was performed using only blood clots without any graft material. In one histomorphometric study of the stability of newly formed bone after elevation of the floor of the maxillary sinus, there was some newly formed lamellar bone embedded in fatty tissue after 10 weeks [26]. The augmented height and area decreased significantly from 2 to 6 weeks [26]. This result might be due to the positive air pressure within the sinus cavity, which promotes sinus pneumatization. The blood clots alone may not withstand this pressure, leading to rapid resorption. To minimize the risk of graft resorption caused by air pressure, bone graft materials were utilized for sinus augmentation. For a certain period following the procedure, the augmented bone height remained stable [27]. This observation suggests that xenograft particles can withstand air pressure, which is known to trigger osteoclastic bone resorption [28]. However, clinical biopsy results indicate that xenogenous graft material exhibits slow resorption or may even remain non-resorbable for up to six years [28]. Since non-resorbable grafts do not transform into new bone, they may not integrate functionally with the surrounding bone tissue [29]. This study aimed to explore an alternative to conventional sinus augmentation methods, addressing their inherent limitations. We investigated the use of a patient’s extracted tooth as a grafting material for sinus augmentation. Since the extracted tooth serves as an autogenous graft, it eliminates the risk of complications at the donor site. To achieve this, the extracted tooth was processed into a demineralized autogenous tooth block. This technique required a smaller volume of graft material compared to traditional methods. A single posterior molar was sufficient for one sinus augmentation. Additionally, it can simplify implant surgery, as only a single block needs to be placed in the sinus. Furthermore, utilizing the patient’s own extracted tooth significantly reduced costs compared to commercially available graft materials [20]. Additionally, our findings indicate that the demineralized autogenous tooth block effectively maintained the augmented space by withstanding the air pressure of the maxillary sinus [30]. The ideal properties of sinus graft materials should ensure biological safety, promote osteoinduction, and provide space maintenance [31]. Demineralized autogenous tooth block bone has been shown to effectively preserve space, thereby preventing pneumatization of the surrounding area. Additionally, there are several reports that demineralized autogenous tooth bone stimulates osteogenesis [32,33]. This osteogenic potential is attributed to the presence of various growth factors, including transforming growth factor-beta (TGF-β), fibroblast growth factor (FGF), bone morphogenetic proteins (BMPs), platelet-derived growth factor (PDGF), and epidermal growth factor (EGF) [34]. Many dentists, when performing a sinus lift using the lateral approach, grind the lateral wall of the maxillary sinus to expose the Schneiderian membrane [35]. In such cases, after surgery, the area should be covered with an additional membrane to prevent soft tissue from growing into the maxillary sinus [35]. In contrast, in this study, a precise osteotomy technique was applied to the lateral wall of the maxillary sinus, and the bony window was completely detached. Therefore, the bony window could be repositioned after the sinus surgery. Through this procedure, the intrusion of soft tissue into the maxillary sinus was prevented, and the bony window acted as an osteoinductive scaffold, promoting new bone formation within the sinus [36]. Additionally, it eliminated the need for membranes, reducing both material costs and the surgical time required for membrane stabilization [36]. A precise osteotomy is crucial for repositioning the bony window accurately. In this study, the use of a piezoelectric device facilitated the surgical procedure. First, the thin saw tip enabled a precise osteotomy of the sinus lateral wall, and it also allowed for easy repositioning of the bony window after the surgery. In addition, this device offers several benefits, including enhanced new bone formation, improved visibility of the surgical site, precise bone cutting, and effective soft tissue protection, which helps prevent arterial damage [37]. This study had two main limitations. First, the retrospective design with a relatively small sample size limits the generalizability of the findings. Second, there was no direct comparison with other graft materials, making it difficult to determine whether demineralized autogenous tooth block bone is superior to alternative options. Future prospective studies with larger cohorts and direct comparisons to other graft materials are needed to validate and expand upon these findings.
Based on clinical and radiographic findings, this retrospective study demonstrates that sinus bone grafting can be successfully achieved using only a single piece of demineralized autogenous tooth block bone. In this study, all 18 patients (25 implants) achieved a 100% implant survival rate during the follow-up period, with no cases of implant mobility or failure. No significant postoperative complications, infections, or sinus-related diseases were observed, even in cases with minor Schneiderian membrane perforation. Radiographically, a significant increase in alveolar bone height and consistent new bone formation around the implants was observed in all cases. Furthermore, the extent of Schneiderian membrane elevation showed a positive correlation with new bone formation, while preoperative bone height and sinus width did not significantly influence the outcome. The findings indicate that demineralized autogenous tooth block bone contributes to a favorable prognosis in sinus augmentation. Therefore, this technique provides significant benefits for both patients and clinicians, offering a biologically safe and cost-effective alternative to conventional grafting methods.
| BMPs | Bone Morphogenetic Proteins |
| CBCT | Cone-Beam Computed Tomography |
| EGF | Epidermal Growth Factor |
| FGF | Fibroblast Growth Factor |
| MISE | Minimal Invasive Sinus Elevation |
| PDGF | Platelet-Derived Growth Factor |
| PRP | Platelet-Rich Plasma |
| TGF-β | Transforming Growth Factor-Beta |
Conceptualization and methodology, D.-S.S.; investigation, data curation, and formal analysis, S.-J.H. and D.-H.K.; writing—original draft preparation, S.-J.H.; validation, interpretation, and resources, H.C.; writing—review and editing, H.C. and D.-S.S. All authors have read and agreed to the published version of the manuscript.
All data available are presented in the study in the Results section of the manuscript.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the institutional ethics committee. The study was approved by the Institutional Review Board of Daegu Catholic University Medical Center Institutional Review Board (Approval IRB No. CR-22-174-L). Before surgery, all patients received an explanation of the procedure and provided written informed consent.
No consent for publication is required, as the manuscript does not involve any individual personal data, images, videos, or other materials that would necessitate consent.
The authors declare that there are no conflicts of interest regarding the publication of this paper. No financial or personal relationships with any individuals or organizations could have influenced the work reported in this manuscript.
The study did not receive any external funding and was conducted using only institutional resources.
Not applicable.
[1] King, E.M.; Schofield, J. Restoratively Driven Planning for Implants in the Posterior Maxilla—Part 1: Alveolar Bone Healing, Bone Assessment and Clinical Classifications. Br. Dent. J. 2023, 235, 706. [CrossRef] [PubMed]
[2] Lam, L.; Ivanovski, S.; Lee, R.S.B. Alveolar Ridge Preservation in Posterior Maxillary Teeth for Reduction in the Potential Need for Sinus Floor Elevation Procedures: A Pilot Study. Clin. Oral Implants Res. 2024, 35, 1568–1584. [CrossRef] [PubMed]
[3] Krennmair, G.; Krainhöfner, M.; Schmid-Schwap, M.; Piehslinger, E. Maxillary Sinus Lift for Single Implant-Supported Restorations: A Clinical Study. Int. J. Oral Maxillofac. Implants 2007, 22, 351–358. [CrossRef] [PubMed]
[4] Zhang, J.; Weng, M.; Zhu, Z.; Li, J. Risk Factors for Implant Failure Following Transcrestal Sinus-Floor Elevation: A Case Report and Literature Review. J. Oral Implantol. 2024, 50, 482–491. [CrossRef] [PubMed]
[5] Tiwana, P.S.; Kushner, G.M.; Haug, R.H. Maxillary Sinus Augmentation. Dent. Clin. N. Am. 2006, 50, 409–424. [CrossRef] [PubMed]
[6] Lafzi, A.; Atarbashi-Moghadam, F.; Amid, R.; Sijanivandi, S. Different Techniques in Transalveolar Maxillary Sinus Elevation: A Literature Review. J. Adv. Periodontol. Implant Dent. 2021, 13, 35–42. [CrossRef] [PubMed]
[7] Giudice, G.L.; Iannello, G.; Terranova, A.; Giudice, R.L.; Pantaleo, G.; Cicciù, M. Transcrestal Sinus Lift Procedure Approaching Atrophic Maxillary Ridge: A 60-Month Clinical and Radiological Follow-Up Evaluation. Int. J. Dent. 2015, 2015, 261652. [CrossRef] [PubMed]
[8] Çelik, O.E.; Ceylan, M.E. Sinus Augmentation Using Caldwell-Luc Technique in the Existence of Ectopic Tooth in the Maxillary Sinus: A Multidisciplinary Approach. J. Craniofac. Surg. 2022, 33, e758–e761. [CrossRef] [PubMed]
[9] Gao, S.; Jiang, Y.; Yao, Y.; Li, S.; Cai, X. Minimally Invasive Techniques for Lateral Maxillary Sinus Floor Elevation: Small Lateral Window and One-Stage Surgery2—A 2–5-Year Retrospective Study. Int. J. Oral Sci. 2023, 15, 28. [CrossRef] [PubMed]
[10] Sohn, D.S.; Lee, J.S.; An, K.M.; Choi, B.J. Piezoelectric Internal Sinus Elevation (PISE) Technique: A New Method for Internal Sinus Elevation. Implant Dent. 2009, 18, 458–463. [CrossRef] [PubMed]
[11] Schlegel, K.A.; Fichtner, G.; Schultze-Mosgau, S.; Wiltfang, J. Histologic Findings in Sinus Augmentation with Autogenous Bone Chips Versus a Bovine Bone Substitute. Int. J. Oral Maxillofac. Implants 2003, 18, 53–58. [PubMed]
[12] On, S.W.; Cho, S.W.; Yang, B.E. A Review of Rare Complications of Maxillary Sinus Floor Augmentation. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 351–356. [CrossRef] [PubMed]
[13] Arias-Irimia, Ó.; Dorado, C.B.; Moreno, G.G.; Brinkmann, J.C.; Martínez-González, J.M. Pre-Operative Measurement of the Volume of Bone Graft in Sinus Lifts Using CompuDent. Clin. Oral Implants Res. 2012, 23, 1070–1074. [CrossRef] [PubMed]
[14] Albanese, A.; Licata, M.E.; Polizzi, B.; Campisi, G. Platelet-Rich Plasma (PRP) in Dental and Oral Surgery: From the Wound Healing to Bone Regeneration. Immun. Ageing 2013, 10, 23. [CrossRef] [PubMed]
[15] Georgakopoulos, I.; Tsantis, S.; Georgakopoulos, P.; Korfiatis, P.; Fanti, E.; Martelli, M.; Costaridou, L.; Petsas, T.; Panayiotakis, G.; Martelli, F.S. The Impact of Platelet Rich Plasma (PRP) in Osseointegration of Oral Implants in Dental Panoramic Radiography: Texture Based Evaluation. Clin. Cases Miner. Bone Metab. 2014, 11, 59–66. [CrossRef] [PubMed]
[16] Rapone, B.; Inchingolo, A.D.; Trasarti, S.; Ferrara, E.; Qorri, E.; Mancini, A.; Montemurro, N.; Scarano, A.; Inchingolo, A.M.; Dipalma, G.; et al. Long-Term Outcomes of Implants Placed in Maxillary Sinus Floor Augmentation with Porous Fluorohydroxyapatite (Algipore® FRIOS®) in Comparison with Anorganic Bovine Bone (Bio-Oss®) and Platelet Rich Plasma (PRP): A Retrospective Study. J. Clin. Med. 2022, 11. [CrossRef] [PubMed]
[17] Kim, E.S.; Kang, J.Y.; Kim, J.J.; Kim, K.W.; Lee, E.Y. Space Maintenance in Autogenous Fresh Demineralized Tooth Blocks with Platelet-Rich Plasma for Maxillary Sinus Bone Formation: A Prospective Study. Springerplus 2016, 5, 274. [CrossRef] [PubMed]
[18] Shavit, E.; Shavit, I.; Pinchasov, D.; Shavit, D.; Pinchasov, G.; Juodzbalys, G. The Use of Tooth Derived Bone Graft Materials in Sinus Augmentation Procedures: A Systematic Review. J. Oral Maxillofac. Res. 2019, 10, e1. [CrossRef] [PubMed]
[19] Choi, H.; Sohn, D.S. Retrospective Study of Maxillary Sinus Augmentation Using Demineralized Tooth Block Bone for Dental Implant. Bioengineering 2024, 11. [CrossRef] [PubMed]
[20] Sun, H.; Yin, X.; Yang, C.; Kuang, H.; Luo, W. Advances in Autogenous Dentin Matrix Graft as a Promising Biomaterial for Guided Bone Regeneration in Maxillofacial Region: A Review. Medicine 2024, 103, e39422. [CrossRef] [PubMed]
[21] Franceschelli, S.; Lagioia, R.; De Cecco, F.; Minetti, E.; Ballini, A.; Panella, V.; Speranza, L.; Grilli, A.; Mastrangelo, F. Biological Evaluation of the Osteoinductive Potential of Dry Teeth after Chemical Demineralization Treatment Using the Tooth Transformer Device. Biomolecules 2023, 13. [CrossRef] [PubMed]
[22] Cho, S.; Min, E.J.; Hwa, S.; Lee, H.; Ko, Y.; Park, J.B. Crestal Approach for Maxillary Sinus Augmentation in Individuals with Limited Alveolar Bone Height: An Observational Study. Medicine 2024, 103, e40331. [CrossRef] [PubMed]
[23] Tawil, G.; Barbeck, M.; Unger, R.; Tawil, P.; Witte, F. Sinus Floor Elevation Using the Lateral Approach and Window Repositioning and a Xenogeneic Bone Substitute as a Grafting Material: A Histologic, Histomorphometric, and Radiographic Analysis. Int. J. Oral Maxillofac. Implants 2018, 33, 1089–1096. [CrossRef] [PubMed]
[24] Mazor, Z.; Gaspar, J.; Silva, R.; Pohl, S.; Gandhi, Y.; Huwais, S.; Bergamo, E.T.P.; Bonfante, E.A.; Neiva, R. Maxillary Sinus Membrane Perforation Rate Utilizing Osseodensification-Mediated Transcrestal Sinus Floor Elevation: A Multicenter Clinical Study. Clin. Implant Dent. Relat. Res. 2024, 26, 1172–1180. [CrossRef] [PubMed]
[25] Moon, J.W.; Sohn, D.S.; Heo, J.U.; Shin, H.I.; Jung, J.K. New Bone Formation in the Maxillary Sinus Using Peripheral Venous Blood Alone. J. Oral Maxillofac. Surg. 2011, 69, 2357–2367. [CrossRef] [PubMed]
[26] Xu, H.; Shimizu, Y.; Ooya, K. Histomorphometric Study of the Stability of Newly Formed Bone after Elevation of the Floor of the Maxillary Sinus. Br. J. Oral Maxillofac. Surg. 2005, 43, 493–499. [CrossRef] [PubMed]
[27] Kim, D.H.; Ko, M.J.; Lee, J.H.; Jeong, S.N. A Radiographic Evaluation of Graft Height Changes after Maxillary Sinus Augmentation. J. Periodontal Implant Sci. 2018, 48, 174–181. [CrossRef] [PubMed]
[28] Fernández, M.P.R.; Gehrke, S.A.; Martinez, C.P.A.; Guirado, J.L.C.; de Aza, P.N. SEM-EDX Study of the Degradation Process of Two Xenograft Materials Used in Sinus Lift Procedures. Materials 2017, 10. [CrossRef] [PubMed]
[29] Yang, Z.; Wu, C.; Shi, H.; Luo, X.; Sun, H.; Wang, Q.; Zhang, D. Advances in Barrier Membranes for Guided Bone Regeneration Techniques. Front. Bioeng. Biotechnol. 2022, 10. [CrossRef] [PubMed]
[30] Sohn, D.S.; Moon, Y.S. Histomorphometric Study of Rabbit’s Maxillary Sinus Augmentation with Various Graft Materials. Anat. Cell Biol. 2018, 51, S1–S12. [CrossRef] [PubMed]
[31] Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26. [CrossRef] [PubMed]
[32] Zhang, S.; Li, X.; Qi, Y.; Ma, X.; Qiao, S.; Cai, H.; Zhao, B.C.; Jiang, H.B.; Lee, E.S. Comparison of Autogenous Tooth Materials and Other Bone Grafts. Tissue Eng. Regen. Med. 2021, 18, 327–341. [CrossRef] [PubMed]
[33] Bao, J.; Fu, X.; Wu, Y.; Yang, S.; Ren, X.; Fang, X.; Yuan, Q.; Xie, Z.; Seriwatanachai, D. The Healing Capacity and Osteogenesis Pattern of Demineralized Dentin Matrix (DDM)-Fibrin Glue (FG) Compound. Sci. Rep. 2023, 13. [CrossRef] [PubMed]
[34] Rodrigues, M.; Griffith, L.G.; Wells, A. Growth Factor Regulation of Proliferation and Survival of Multipotential Stromal Cells. Stem Cell Res. Ther. 2010, 1, 32. [CrossRef] [PubMed]
[35] Hamed, H.A.; Shaaban, A.M.; Melek, L.N. Evaluation of Trephine Osteotomy Technique in Direct Sinus Lifting with Simultaneous Implant Placement. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101347. [CrossRef] [PubMed]
[36] Kim, J.M.; Sohn, D.S.; Heo, J.U.; Moon, J.W.; Lee, J.H.; Park, I.S. Benefit of the Replaceable Bony Window in Lateral Maxillary Sinus Augmentation: Clinical and Histologic Study. Implant Dent. 2014, 23, 277–282. [CrossRef] [PubMed]
[37] Hennet, P. Piezoelectric Bone Surgery: A Review of the Literature and Potential Applications in Veterinary Oromaxillofacial Surgery. Front. Vet. Sci. 2015, 2. [CrossRef] [PubMed]
We use cookies to improve your experience on our site. By continuing to use our site, you accept our use of cookies. Learn more